“We will be able to reopen completely our societies, and COVID-19 will become a regular flu.”
By Rev. Fr. Nicanor Pier Giorgio Austriaco, O.P., Ph.D., S.Th.D., M.B.A.
Professor of Biological Sciences & Professor of Sacred theology
University of Santo Tomas, Philippines
Thank you po, Mr. President, and I’m a Filipino Catholic priest-scientist and I’m speaking to you from the United States.
So this evening I’ve been asked to brief you po on the Omicron variant of SARS-CoV-2 and I would like to highlight some of the most recent clinical data that we have obtained from South Africa.
I would like to begin by just giving you a perspective on the current assessment on the COVID-19 pandemic in the Philippines. I’m a molecular biologist, so I would like to give you a sense of my perception of the pandemic.
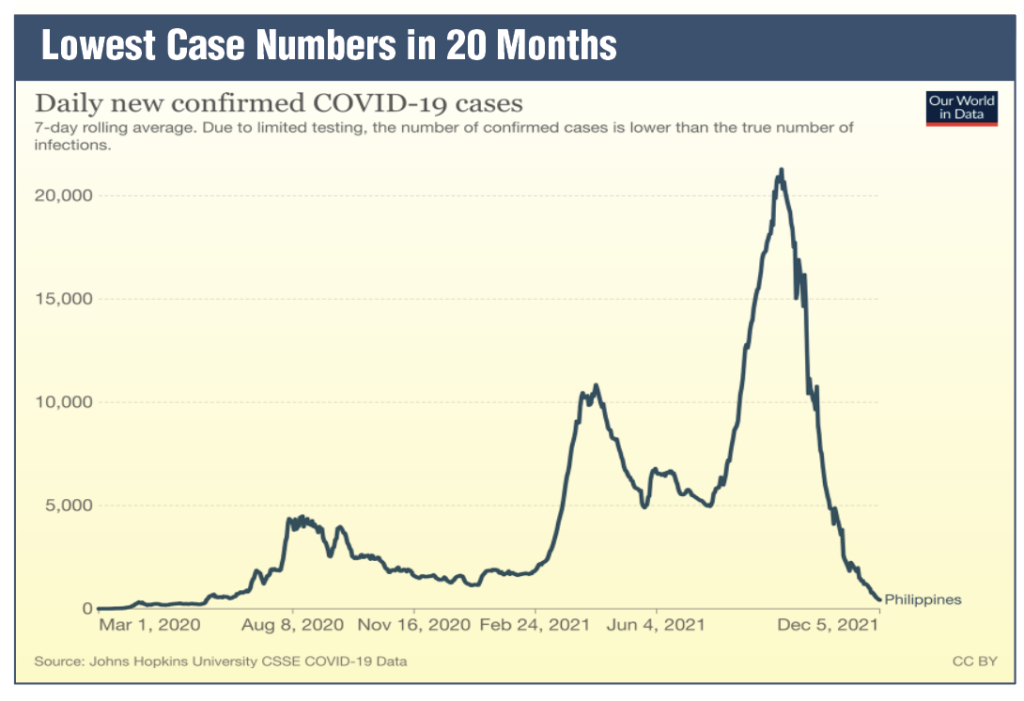
Lowest case numbers
As you pointed out at the beginning of the Cabinet meeting, we are experiencing the lowest case numbers in 20 months, with an average of about 500 cases per day. I would like to contrast that with here in the United States. Yesterday (Dec. 5) we had 120,000 new cases and the United States is only three times the size of the Philippines (see above Lowest Case Numbers in 20 months graph).
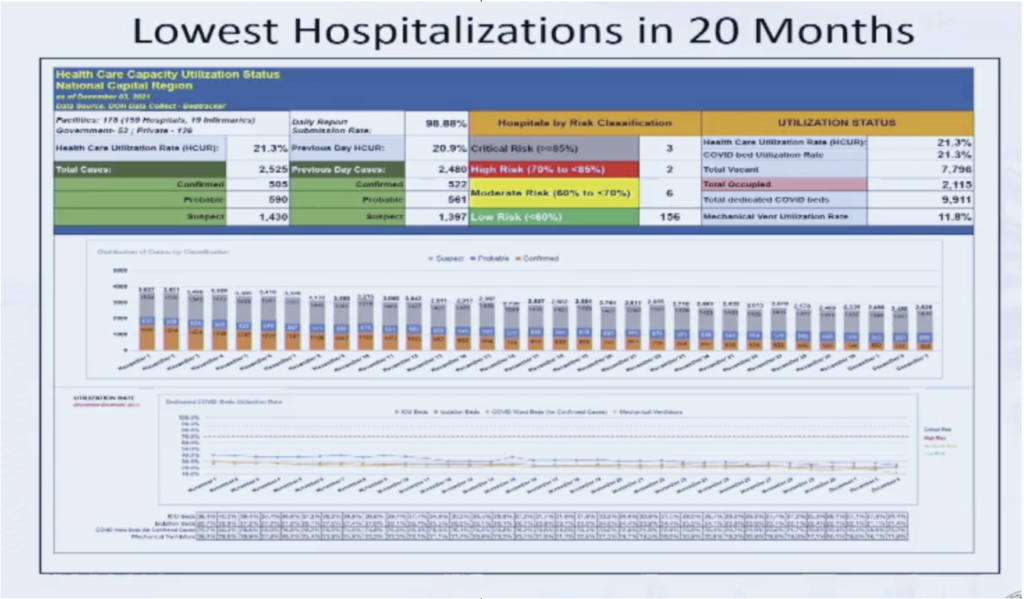
What is also striking is that these are — we are also experiencing the lowest hospitalization numbers in 20 months. Earlier today, Makati Med announced for the first time during the pandemic, they have no COVID-19 patients in their hospital. And this is typical of many hospitals throughout our beloved country. (see above Lowest Hospitalizations in 20 months graph)
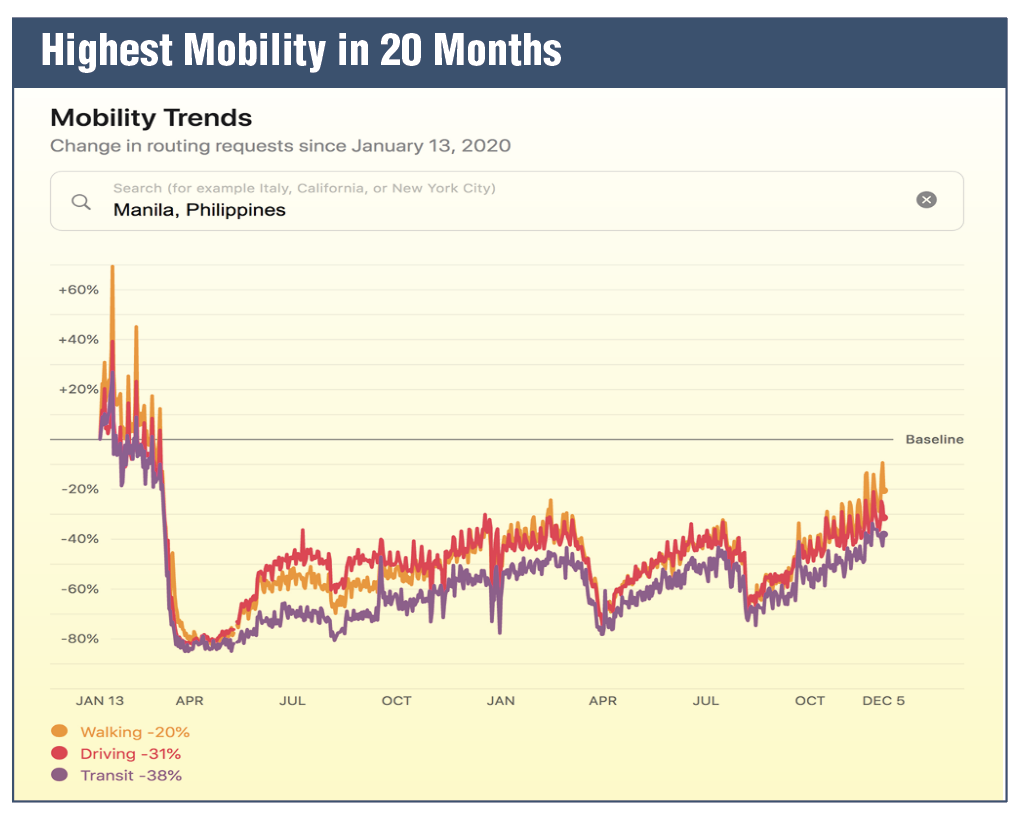
But this is also interesting because we are experiencing the highest mobility in 20 months. So this is a graph from Apple Mobility, and the higher the curves, the more people are moving around. And what you can see this is the mobility trends from the NCR. What you can see is that — most — many of our people are moving around now, the most in 20 months since the beginning of the pandemic and the lockdown in March of 2020 (see page 27 Highest mobility in 20 months graph).
And so as a biologist, this is the question: we are currently with Delta, the most infectious variant in the past 20 months, the highest mobility levels in the past 20 months, more and more of our kababayans are moving around, and yet we are experiencing the lowest levels of cases and hospitalizations in 20 months.
Substantial population immunity
And so what these three mean together is that it suggests that we have attained substantial population immunity from natural infections and vaccinations in the urban areas of the Philippines because the pandemic has raged and spread primarily in our cities and in our first class municipalities. And so the fact that the virus is struggling to find new Filipinos to infect, suggests that we have attained substantial population immunity.
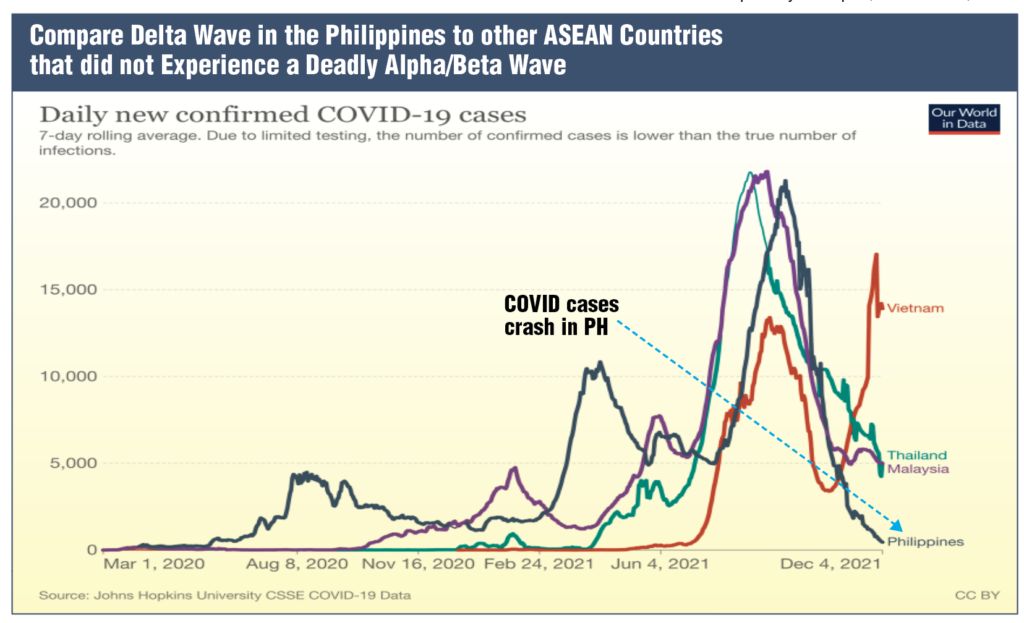
This is to compare the Philippines with three of our ASEAN neighbors. So if you look, the lowest graph is the Philippines and we are at 500 cases per day. You can see Thailand and Malaysia had the Delta surge earlier than we did, but their — their surge has not been able to crash. So at this time, Thailand and Malaysia are still experiencing 5,000 cases per day (see page 27 Compare Delta Wave in the Philippines to other ASEAN Countries graph).
Now contrast that with Vietnam. Vietnam also had a Delta peak. Unfortunately, the Delta peak has resurged and Vietnam is still experiencing significant numbers of COVID-19, 15,000 or so per day.
Now the reason why these four different countries have experienced different pandemic curves is probably because as you can see the Philippines experienced — unlike these three other countries substantial waves of previous variants. So the — especially the Alpha, Beta variant, which struck our beloved country in March and April of this year.
And so combining the vaccinations and the natural immunity, what you are seeing here is that many of our cities where the pandemic tends to focus are now — are now stable enough to prevent transmission.
I just wanted to highlight this graph from the Financial Times, which illustrates the population immunity in different countries in Europe. On the left-hand side, you have Spain, which has about 90% of eligible population vaccinated. And the NCR and many of our urban cities have very similar vaccination levels (see above Population Immunity Protects Against Future Waves of COVID-19 graph).
Number of deaths
And what you can see on the left-hand side, if you focus on the red curve, the red curve is the number of deaths. And what you can see is that the higher the population that is protected, the smaller the red curve. And across Europe, what you will notice is as the vaccination levels drop, the red curve begins to explode because the current wave that is flowing through Europe which is Delta-driven is still quite significant.
At this time, given our significantly high numbers of vaccination, not only in the NCR but in many of our cities. Secretary Vince just sent me the numbers for our cities and our first class municipalities, and many of them are quite significant, above 70% for the first dose at least. What we are seeing here is that at least the NCR, with nearly a hundred percent protection of the adults and with the increasing numbers of our teenagers, is probably going to be robustly protected against the future surge.
We will now move to the COVID-19 Omicron threat to the Philippines and I would like to begin as a biologist just to explain what Omicron is.
Here, you see the best animation of the SARS-CoV-2 virus. And on the surface of the virus, you see about 25 spike proteins. And these spike proteins are important because the virus uses the spike protein as a key to enter the cells of our body.
So for the duration of the pandemic, we had four important variants of concern: Alpha, Beta, Gamma, and Delta. Notice that we
experienced Alpha, Beta, and Delta surges in the Philippines but not really a significant Gamma surge.
We now have Omicron, and this is the — so this makes the 5th of the important variants of concern, and the most significant change is that this virus — this version of the virus has 50+ mutations.
Let me explain. So different variants have different spike proteins. It is the same COVID-19 virus, it’s the same SARS-CoV-2 virus. But different variants have different spike proteins.
And what you can see here is that comparison of the spike protein on the left of the Delta variant and the spike protein on the right of Omicron. Red indicates change, and as you can see there are a few red spots in Delta. But on the right, with Omicron, there is significant red, which means that the shape of the spike protein is different (see above COVID-19 Delta and Omicron variants).
And the reason that this is important po is because the antibodies in our blood recognize the shape of the spike protein. And so, if the shape changes dramatically, this could mean the trans — that the virus is able to escape the immune protection that we have either from a previous infection of COVID-19 or from vaccination.
So, what I would like to go over now is the clinical data that is coming out of South Africa. So, this is the first graph from December 2nd, so it’s only four days ago.
And what you see on the left-hand side po is the daily cases comparing the Omicron wave with the previous waves that were experienced in South Africa.
So the South Africa had a Delta wave, a Beta wave, and the first Wuhan wave, very similar to the Philippines. And what you can see that is most striking po is that the red line is very sharp and it’s going up very quickly, which suggests that the Omicron wave is exploding in a way that is faster than the Delta or the Beta waves that we experienced in the past.
The middle graph shows you the positivity rate. And again, what you are seeing here is the Omicron variant is exploding in South Africa. But what is most important po is on the right.
On the right, you see the hospitalizations in South Africa. And what you see is despite the accelerating numbers of cases of Omicron, the hospitalizations are on track. They are not rising faster, very similar to the other waves of the variants in South Africa.
This is the preliminary data that was published on Saturday (Dec. 3) po. What we are looking at here now is the relative risk…
So, on this graph, if you are a 100% — if the red line was 100%, then the risk is comparable between an unvaccinated and a vaccinated Filipino (see Reinfections with COVID-19 graph on the left).
What you can see is that the Delta wave had a 9% relative risk and we can see that the Omicron wave is three times higher than the Delta wave. So it is true that the preliminary data coming from South Africa suggests that the Omicron variant is more transmissible amongst vaccinated individuals.
But it is really important to focus on hospitalizations po. So if you look at the hospitalizations… This is a screen grab from a presentation from the Department of Health in South Africa, from the province of Gauteng, which is the hotspot for the Omicron explosion that is currently taking place. (see below Data on Hospitalization of Omicron Patients visual)
What you can see is that the preliminary data suggests that 10 times more unvaccinated individuals are being hospitalized as compared to vaccinated individuals.
This is incredibly hopeful especially since as I highlighted before, because of the NCR Plus 8 strategy, our cities and first class municipalities, which is the target for Omicron when it arrives in the Philippines, are highly vaccinated.
This is data from the Tshwane District, South Africa from three days ago po. So this is the most recent data that we can get on the Omicron.
What you can see from a few days ago is that this district in South Africa is experiencing a dramatic surge of COVID-19. They are experiencing 3,000 cases per day on the 3rd of December. On the right, you see that many of the hospitalizations are still — are of people 50 years and below.
Despite the number of COVID-19 positives, however, the Omicron hospitalizations are quite low. So you have only something to the effect of 42 to 29 hospitalizations despite the thousands of individuals who are testing positive for COVID-19.
What is important is that if you look at the numbers of the people who were hospitalized, what is so amazing about the Omicron is that only — is that 70% of them do not need oxygen po. And this is very different from the Delta experience that we experienced throughout the world and in the last few months in the Philippines. So, we have 31% require oxygen; 70% do not require oxygen.
And what is striking is that 10 of the 11 people who needed oxygen were unvaccinated. And again, what this suggests is that if you are vaccinated, this will protect you against severe disease and hospitalizations even with Omicron, which is good news for us.
So there are three important questions that the scientists of the world are waiting for: Is the Omicron variant more transmissible? It is likely po that it is more transmissible. Is the Omicron variant more immune
evasive?
Probably po. The initial data seems to look like that. Is the Omicron variant more deadly? And this is the good news po, it’s probably less deadly than Delta.
I have to point out po that this is preliminary data and we are waiting for data from the older populations in the global north because there are not many lolos and lolas in South Africa. And so most of the patients that we are seeing in the hospitals of South Africa are relatively young.
We still do not know po what will happen when it — when Omicron begins to spread in the northern part of the world where more of the population are older. I also have to point out that hospitalizations are lagging indicator.
It usually takes a week or two weeks after a surge to see the
hospitalizations. But the data from South Africa is very hopeful, especially since they have already been dealing with the surge for at least a week or two and the hospitalizations do not seem to be dramatically increasing po.
Based on this, I would like to suggest the following for preparations for the arrival of the Omicron variant in the Philippines. First, there is no need to panic. We — let us celebrate Pasko. This is the best time in 20 months for the entire country.
You know, I am so proud to be a Filipino because I boast of this. Here in the United States, I say we have 500 cases po yesterday compared to 120,000. The positivity rate is less than 2%. This is some of the best numbers in the world.
And so this is not the time to panic. It is the time to be careful. We have to prepare. But we also have to celebrate especially since this is Christmas. We must prepare the hospital infrastructure and increase healthcare workers staffing capacity po. Because in the Alpha and Delta surges it was clear that we had nursing shortages, especially in the NCR.
We have to continue to vaccinate and to boost our kababayans to build and maintain population immunity. This is really important po because the experience of Israel and other countries that vaccinated early showed that it is important to boost at the appropriate time to maintain population immunity.
We must increase the population immunity around our international gateways. Omicron will enter through an airport most likely.
And so what we have to do is we have to build a wall of vaccinated Filipinos around these airports. Because once Omicron arrives, it will try to spread into the Filipino population.
And if the Filipinos around the airports po — and this was the rationale strategy for the NCR Plus 8 — are heavily vaccinated, then it doesn’t matter if there is an OFW who returns home. Because even if this person is able to enter the community, the virus will struggle.
My university po in the United States has a 98% vaccination coverage in our staff and our students. And every time a student goes out and gets a COVID-19 when he returns, no one else gets sick po. The — and we are dealing with Delta.
It is struggling because of the high numbers of vaccination. The population is protected. However, I — for our kababayans who are watching me, I must urge you to get vaccinated because Omicron, when it arrives in the Philippines, will find every unvaccinated Filipino. And you will get sick, and even though it is mild, it is still, it is still COVID-19.
And we do not want to put ourselves and our beloved family members, especially our lolos and lolas into — we do not want to risk them, to risk their lives and their well-being and their livelihood, especially at this time.
I would like to end my presentation po with a short discussion of the antiviral drugs.
The importance po of emphasizing the antiviral drugs is that they are equally effective against all variants of SARS-CoV-2. One of the things is that, you know, the vaccines depend upon the variants. But the anti-viral drugs are equally effective.
And the reason for this po is that these drugs work on the virus, they kill the virus once the virus enters the human cells. And so, the outside of the virus will change with the different variants but the inside po will not change.
And so Pfizer’s paxlovid, Merck’s molnupiravir will be effective. And this is the most recent data on the anti-virals that’s coming out of Merck and Pfizer. I know that Merck’s molnupiravir has already been authorized for compassionate use in the Philippines. And I thank Secretary Duque and the DOH for that.
What you are seeing here po is that when in clinical trials with high-risk patients — lolos, lolas with underlying comorbidities — the Merck antiviral was able to prevent 30% of the high-risk patients from entering the hospital.
But look po at Pfizer, 90% protection for high-risk patients from entering the hospitals. In comparing deaths… So both of these drugs were able to prevent deaths as compared to non-drugs which had nine for molnupiravir and seven for paxlovid.
And what this means po is that if a Filipino gets COVID and is at high risk, what we would have to do if we have these drugs is we have to give this Filipino, our kababayan, 10 pills. Two every day for five days po. That is all that is needed, and we will be able to prevent him from entering the hospital. He will be sick at home but it will be mild. He will not be hospitalized.
Now, the cost here in the United States is $700 for the entire 10 dose — 10 doses and paxlovid, [$]500. But I know that Merck has already opened its license for the manufacturing of generic versions and I know that the Philippines will have access to this.
So the way out of this pandemic is through vaccinations which we are doing now po.
And we must continue to do that to maintain our immunity, especially with the Omicron threat. And we now have to also focus our efforts on procuring anti-viral drugs.
This combination po will transform pandemic COVID-19 into endemic COVID-19, where we will be able to reopen completely our societies, and where COVID-19 will become a regular flu.
And so I thank you po for your service to our beloved country. I always end with one more slide to Our Lady. Thank you so much and God bless you po.